Contact Lenses & Spectacles
Spectacles and Soft Contact Lenses
In the early stages of the condition, spectacles are usually successful in correcting the myopia and astigmatism associated with the keratoconus and provide sufficient vision.
 As the condition advances, the cornea becomes highly irregular and vision is no longer adequately corrected with spectacles and contact lenses must be considered.
As the condition advances, the cornea becomes highly irregular and vision is no longer adequately corrected with spectacles and contact lenses must be considered.
Soft lenses can be used for mild keratoconus and sports, especially contact sports. But as they conform to the irregular shape of the cornea, they offer limited improvement in vision in more advanced keratoconus.
Newer soft lens designs with a thickened central optic zone and thinned periphery can provide good comfort and vision. These need to be made from highly oxygen permeable materials to preserve eye health and avoid neovascularization.
Soft lenses are also used in piggyback lens systems which employ a soft lens under a rigid gas permeable lens which provides vision correction.
Emergency spectacles should be kept by all keratoconus patients to wear before inserting and after removing contact lenses to reduce contact lens wearing times. Spectacles are also useful for plane travel (especially long haul) as plane cabins have a dry, bacteria laden environment.
Contact Lenses
Rigid contact lenses (RGPs) are the most common contact lenses prescribed for keratoconus to provide optimal visual acuity. They offer the best long term, non surgical solution for most patients with moderate to advanced keratoconus.
Most patients can generally wear RGPs all day with good comfort and stability, excellent vision and clear eyes. Although these can be uncomfortable initially due to the sensitivity of the cornea, patients gradually get used to wearing them and after 2-4 weeks should no longer be aware of them.
The long term success of RGPs generally depends on whether they are fitted by a specialist contact lens fitter for keratoconus. It can take a number of visits and adjustments to achieve the right fit so patience is required by both contact lens fitter and patient. There are very few of these specialist contact lens fitters and most are located in the major capital cities.
Signs of a poor fit are discomfort, instability (lens popping out when you turn your eyes or head, blink etc) and eye redness. Patients must seek an immediate review and refit should they experience these symptoms as a poorly fitted contact lens can cause long term and permanent damage to the cornea.
Regular reviews (6-12 monthly) are also essential to check that there has been no progression of the keratoconus, to check that the rigid gas permeable contact lenses are still fitting well, are in good condition, that the vision is stable and that the eye is healthy.
Types of Lenses
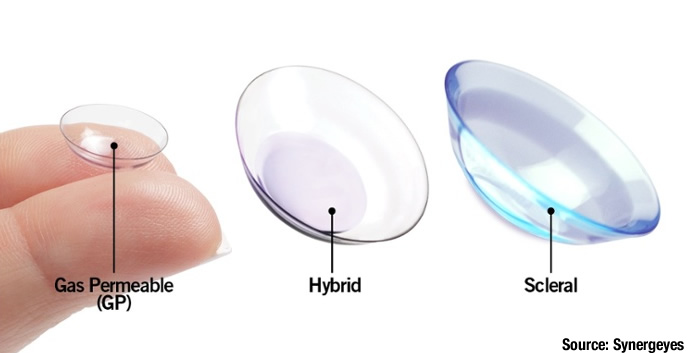
There are a number of different types of contact lenses for keratoconus.
Standard RGPs traditionally had a diameter of 7.5 - 9 mm. These days there is a trend towards prescribing larger lenses for keratoconus to improve patient comfort, assist with lens centration and provide a larger area of vision. These lenses have a diameter of between 10 - 16 mm which can make them a little harder to insert and remove.
RGPs have many advantages over soft lenses:
- made with high oxygen permeable silicone to provide more oxygen to the front of the eye than hydrogel soft contact lenses (although newer silicone hydrogel lens are becoming comparable).
- sharper vision as they maintain their shape on the cornea.
- can last 12-24 months with good care and don't rip or tear.
Some disadvantages include:
- adaptation time may be several weeks, building from a few hours at first.
- susceptibility to dust, grit and sand especially on windy days which can cause extreme discomfort and may be difficult to dislodge.
- higher initial and replacement cost than soft lenses, especially for complex designs.
- longer replacement times of up to a week which may necessitate users buying a spare pair.
Mini sclerals are even bigger than large RGPs - 16.5 mm - and sit on the sclera or white part of the eye. They are well suited to people working in a dusty environment or engaging in sports.
Mini sclerals have certain advantages over smaller RGPs:
- improved comfort as they should not touch any part of the highly sensitive cornea if fitted properly
- stable vision as they maintain their position better than a smaller RGP
- should last at least two years with good care as they are about twice the thickness of a normal RGP
- less likely to dislodge as they are larger, sit under the eyelids and fluid forces hold them in place
- reduce allergy symptoms as the tight seal around the lens acts as a barrier to allergens
- less dryness as mini sclerals must be filled before insertion with saline solution or artificial tears. This makes them useful for patients with dry eye or ocular surface disease
- less foreign bodies such as dust, grit and sand can enter the sealed environment
Some disadvantages include:
- high initial cost which can be between $1,500-$2,500 a pair including fitting fees.
- less tear exchange than a RGP lens which can compromise oxygen and nutrient flow to the corneal surface. Correct fitting to ensure adequate lens edge clearance is therefore imperative.
- sealed system can mean the lenses are tricky to insert and remove
Despite the difficulty in fitting and managing these minisclerals, they are worth trying as they generally offer a last option for more advanced keratoconus patients who cannot be fitted with smaller lenses. As such, they provide a possible alternative to a corneal transplant.
Hybrid lenses (Synergeyes) offer another alternative for advanced keratoconus. These are made with a rigid central portion (to improve vision) attached to a peripheral soft skirt (to improve comfort). The latest types are made from a more durable and gas permeable material than previous iterations (Softperm). Although a comfortable alternative to RGPs, they are very expensive and need to be replaced every 6 - 12 months.
FAQs
Are contact lenses for everyone?
It depends. Although rigid contact lenses, provide the best vision correction for keratoconus, not everyone may be suited to wearing them. People with poor spectacle vision in one eye but normal vision in the other, may not bother with correction for their bad eye unless they need a high level of three dimensional vision for activities such as ball sports.
The age of patient, their ability to manage contact lenses and their general health are also factors to consider.
Am I really allergic to rigid contact lenses?
Probably not. The success rate for RGPs amongst keratoconus patients is around 85%. Most allergic reactions or rigid lens failures or rigid lens dropouts arise from poor contact lens fits by inexperienced practitioners.
The only alternative to rigid contact lenses for most people with keratoconus is surgery - notably corneal transplantation - so it is worthwhile finding a specialist contact lens fitter for keratoconus.
Can wearing rigid gas permeable contact lenses "cure" my keratoconus by flattening out my irregular cornea?
No. Rigid gas permeable contact lenses improve vision by covering the irregular cornea with the regular focussing surface of the contact lens. The lens fitting is carefully designed to lightly rest on the corneal surface to allow all day wearing times and maximum comfort. Fitting a substantially flatter than recommended contact lens curve can significantly flatten the corneal shape, especially in a thin keratoconic cornea, however the corneal irregularity that causes poor quality vision is still present. Also the effect is only temporary and after removing the lens, the cornea gradually returns to its previous irregular shape.
Can wearing rigid gas permeable lenses make my keratoconus worse?
No and Yes.
No - The "perfect fitting" contact lens will have even pressure across the central area of the cornea with enough lift at the edge to allow the lens to move freely and also permit adequate tear flow under the lens. As a keratoconic cornea has an irregular shape, "a perfect fitting" is often impossible to achieve. The final contact lens shape often has to become a compromise of trying to minimise any areas of hard pressure. The more advanced the keratoconus the more difficult this to achieve. A well-fitted lens, even with very advanced keratoconus will not cause an increase in the rate of keratoconic changes in the cornea. Occasionally a lens has to be fitted flatter than recommended to preserve adequate vision and these eyes need to be monitored regularly to ensure the contact lens fitting does not increase corneal scarring.
Yes - Flat fitting lenses with excessive pressure on the elevated and thin cornea have been associated with increased rates of corneal scarring. This situation can arise from a practitioner prescribing an inappropriate contact lens shape. It also can occur when there has been a significant increase in the corneal curvature over time and the patient continues to wear a contact lens design that was fitted when the cornea was flatter. The result is often a lens that is highly unstable and can pop out, even a few times per day. This type of lens also has intense central pressure on the thin cornea. If this lens is worn for months or years, scarring in the cornea can often be seen in the area of hard pressure.
Reduced vision from excessive corneal scarring is one of the major causes why patients finally agree to have a corneal transplant. Sometimes it can be difficult to determine with certainty if the contact lens fitting has caused the scarring or the scarring would have occurred anyway with the natural progression of the keratoconus. Certainly all experienced practitioners will try and minimise the central pressure of the contact lens on the cornea, to preserve vision and avoid any increase in corneal scarring. It also emphasises the need for regular reviews, usually every 6 - 12 months, to make sure that the contact lens fitting is still as good as possible.
Poorly fitted contact lenses often lead to three undesirable outcomes.
- Uncomfortable contact lenses can convince patients that rigid gas permeable contact lenses are always uncomfortable and they may resist future attempts to accept them as a solution for better vision.
- Patients unable to tolerate an uncomfortable rigid gas permeable contact lens may stop wearing lenses and attempt to function with poor vision. This can seriously impact on their ability to study, work and engage in sporting activities. It can create unnecessary hardship and even endanger themselves and those around them, Â e. g. driving without lenses when they have an endorsed license, operating dangerous equipment or increased risk of falls and household accidents etc.
Inability to function normally, often leads to loss of self-confidence and depression. - Frustration with the unreliability of rigid gas permeable contact lenses, patients may seek unnecessary surgical solutions (Intacs, intra ocular lenses, corneal transplant).
Can I sleep in my rigid gas permeable contact lenses?
No. Patients who need rigid gas permeable contact lenses on a daily basis for the best quality vision, risk serious eye infections leading to possible blindness if lenses are kept in when sleeping. Even if a serious infection does not develop, the eyes can develop significant redness and irritation and that can result in reduced wearing times and reduced vision.
Even cat napping is not recommended as the eyes can become dry and irritated. The best solution is to remove the lenses, clean with a daily cleaner and soak them in fresh conditioning solution and reinsert them after the sleep.
If you wake up with the lenses in you eyes, insert some lubricating drops to loosen the lenses and massage the lenses through the lids to make sure they are mobile. Then remove the lenses, and seek a consultation if you eyes are very red or irritated to make sure the eyes have not been damaged. Don't resume wearing the lenses until your eyes are clear and comfortable.
With thanks to
Richard Vojlay BSc Optom LOSc, FACO, PGCertOcTher
Shonit Jagmohan BOptom (Hons), FIAO
Richard Lindsay BSc Optom MBA, FAAO, FCLSA, FACO
Mark Koszec BOptom (Hons), M.Optom, Grad Cert Oc.Ther (UNSW)